Tpa Clot Dissolver
DEAR DOCTOR K:

UPA (urokinase-type plasminogen activator) and tPA (tissue-type plasminogen activator), the drug that is the only approved treatment for acute stroke, have similar names, because they both act biochemically to activate plasmin, which directly dissolves blood clots. “We are finding that uPA and tPA do very different things in the brain. This alternative may benefit patients when treatment cannot begin within three hours after stroke symptoms started or when initial tPA treatment has not been sufficient to dissolve the blood clot. The local administration of tPA can occur up to six hours after the onset of stroke symptoms. The decision to use tPA or other clot-busting drugs. This study will test the effectiveness of low-dose recombinant tissue plasminogen activator (rtPA, or alteplase) in dissolving blood clots in deep leg veins. Alteplase is used to clear blood clots in coronary arteries in patients having heart attacks.
My father recently had an ischemic stroke. He was treated with tPA and has now fully recovered. What is tPA? And how does it work?
DEAR READER:
The most common kind of stroke is called an ischemic (is-KEY-mic) stroke: an artery supplying the brain becomes blocked by a blood clot. The part of the brain supplied by the artery needs the nutrition provided by a constant supply of blood. When that supply is interrupted, brain cells can die, taking with them the ability to move, speak, feel or think.
When a stroke occurs, immediate treatment is crucial. The sooner treatment starts, the better the chance of limiting disability or brain damage — or preventing death.
As soon as doctors diagnose an ischemic stroke, they must determine whether a clot is still blocking an artery. If so, there are drugs to dissolve the clot. Tissue plasminogen activator (tPA) is one of the main drugs used to dissolve clots. It is made naturally by the body, but unfortunately, when a clot suddenly blocks an artery, the body doesn’t make enough tPA to dissolve the clot.
However, tPA produced in the form of a medicine can be given through a thin tube in the arm or a tube threaded through the blood vessels directly to the site of the blockage. High concentrations of tPA build up at the site of the clot, making it dissolve. (I’ve put an illustration of how tPA works to restore blood flow to the brain below.)
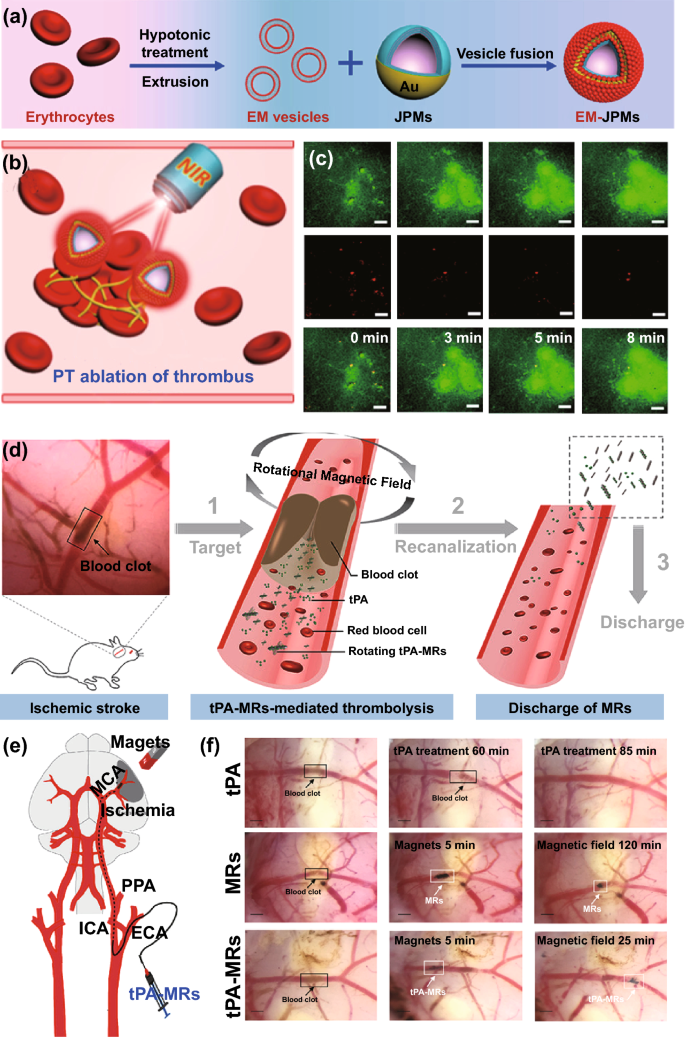
How clot-busters workThrombolytic drugs such as tPA are often the first line of defense in treating some forms of ischemic stroke. The stroke occurs when fibrin strands in the blood trap blood cells and platelets, forming a clot in an artery to the brain (A). The drug breaks up the clot by helping generate the enzyme plasmin, which digests the fibrin strands, restoring blood flow (B). |
Dissolving a clot won’t help the brain if it’s done too late. The phrase doctors use is, “Time is brain.” To be effective, tPA should be administered within 4 1/2 hours after the start of the stroke. When used appropriately, tPA can produce dramatic recovery within hours.
But clot-dissolving drugs also carry risks, and tPA can cause excessive bleeding — which can lead to death. The more time that passes between the start of the stroke and the administration of tPA, the greater this risk.
Clearly, doctors must exercise great caution when deciding whether to use tPA. When possible, this decision is best made by a skilled medical team headed by a stroke specialist.
If doctors rule out tPA, they will likely give an antithrombotic, or anticoagulant drug, such as heparin, to prevent more clots from forming.
When I was a young physician, there was very little we could do for people with ischemic strokes. We knew what the problem was — a clot had blocked a major artery in the brain — but we just had no way of dissolving it.
It took medical research to figure out how clots form and dissolve. Then the huge research breakthrough called recombinant DNA technology allowed us to make large amounts of natural substances like tPA. Without this research, most of it supported by your tax dollars, we would not have tPA, human insulin, or many other life-saving medicines. Think about that when you read about cuts in funding for medical research.
Tpa Clot Buster
This study will test the effectiveness of low-dose recombinant tissue plasminogen activator (rtPA, or alteplase) in dissolving blood clots in deep leg veins. Alteplase is used to clear blood clots in coronary arteries in patients having heart attacks. Blood clots can develop in the deep leg veins causing pain and swelling and may break loose and lodge in the lungs. Current routine treatments use anticoagulants such as heparin stop the clots from enlarging and prevent clots from moving to the lung but do not reliably dissolve clots in the leg.In an earlier study we showed that rtPA could be used to actually dissolve the clots. This study will determine whether lower doses of rtPA can dissolve clots with fewer bleeding complications than the current higher-dose regimens.
Clot Dissolvers Thrombolytics
Patients 18 years of age and older who have blood clots in a deep vein of the pelvis or leg may be eligible for this study if they have had symptoms for 14 days or less and if they have never had clots in their deep veins before.
Participants are admitted to hospital for up to 5 days. On the first treatment day, the patient has a venogram to show the location of the clots. The radiologist injects an x-ray contrast material into a small vein in the foot and watches the dye by x-ray as it moves up the leg, revealing the clot(s). A catheter (plastic tube) is then inserted into a vein either behind the knee, in the groin, or in the neck, and advanced until it reaches the clots. When the catheter is in place, rtPA is injected while the radiologist watches the vein under the x-ray image. The amount of rtPa needed will depends on the size of the clot. Up to five venograms may be done if the clot requires the maximum four rtPA treatments allowed in this study. During the treatments, patients receive standard doses of heparin, given continuously by vein, After completion of treatments, anticoagulation is continued through use of a low molecular weight heparin (usually enoxaparin) given by subcutaneous injection as a transition medication during conversion to anticoagulation with warfarin ( also known as coumadin), another blood thinner, taken by mouth. Patients continue taking warfarin for 6 months.
During thrombolytic therapy, blood samples are drawn shortly before the first dose of rtPA and at five time points afterward to measure the rtPA in the circulation and other factors that indicate whether the rtPA is affecting clotting ability. Blood also is drawn at least once a day to monitor heparin levels.
Tpa Clot Dissolver
To evaluate the impact of treatment on the function of the leg, patients return to the Rehabilitation Medicine Department and Radiology department at about 6 weeks (4 to 8 week ) and 6 months for clinical and imaging evaluation of impact of therapy on venous function.
Natural Clot Dissolvers
The objectives are to determine how well this treatment will restore venous function and whether this can be done safely- without causing bleeding complications, which have been the main risks of previous thrombolytic treatments.